A Comprehensive Guide to Gingivitis — The First Stage of Gum Disease
Gingivitis is a pervasive oral health condition affecting millions globally. Characterized by plaque accumulation on teeth and gums, this disease can lead to significant serious dental health complications if neglected. Left untreated, it potentially causes permanent damage to your oral structures.
At Wright Perio & Implants, San Clemente periodontist, Dr. Raymond L. Wright Jr., and our dedicated dental team are committed to patient education and personalized treatment strategies. To schedule your comprehensive dental evaluation, contact our South Orange County dental practice at (949) 361-4867.
What Is Gingivitis?
Gingivitis represents the initial phase of gum disease, targeting the tissues surrounding and supporting your teeth. It develops through plaque buildup—a sticky bacterial film forming on teeth and gums during eating and drinking. When not eliminated through regular, good oral hygiene, this plaque can calcify into tartar, requiring professional dental intervention.
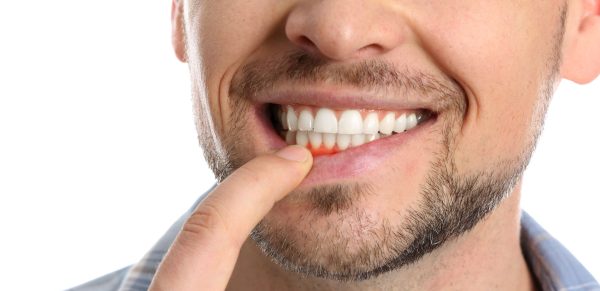
The bacterial organisms within plaque can trigger gum irritation, resulting in redness, swelling, and easy bleeding. Without proper treatment, gingivitis can progress to early periodontitis, compromising your oral health.
Symptoms of Gingivitis
Gingivitis develops through a complex inflammatory process triggered by bacterial plaque accumulation. As harmful bacteria proliferate along the gum line, they initiate a cascade of physiological responses that manifest as distinct symptoms:
Redness
The body’s immune response to bacterial plaque causes increased blood flow to gum tissues, resulting in vasodilation. White blood cells rush to the area, creating a distinctly red or reddish-purple appearance that differs from healthy pink gums. This inflammatory response is the body’s initial defense mechanism against bacterial invasion, making the gum tissues visibly inflamed and discolored.
Swelling
Bacterial toxins and immune responses cause fluid accumulation in gum tissues. Inflammatory mediators increase tissue permeability, promoting fluid retention and creating puffy, enlarged gum surfaces. The swelling represents the body’s defensive strategy to isolate and combat the bacterial infection, causing noticeable changes in gum texture and volume.
Bleeding Gums
Bacterial infections weaken blood vessels in gum tissues, making them extremely fragile. The inflammation damages cell walls, causing blood vessels to rupture and bleed easily during routine oral hygiene. Even gentle brushing or flossing can trigger bleeding, as the gums become hypersensitive and vulnerable to the ongoing bacterial assault.
Tender or Sensitive Gums
Inflammatory responses dramatically increase nerve sensitivity in gum tissues. Bacterial toxins and immune compounds stimulate nerve endings, creating heightened sensitivity to touch, temperature, and pressure. Patients experience discomfort ranging from mild tenderness to sharp pain as the inflamed tissues put pressure on nerve receptors.
Bad Breath
Anaerobic bacteria proliferating in inflamed gum tissues produce volatile sulfur compounds. These bacteria metabolize food particles and dead cells, creating a persistent, distinctive odor that resists standard oral hygiene practices. The bad breath directly results from the bacterial ecosystem developing within the infected gum tissues.
Receding Gums
Chronic inflammation progressively destroys the connective tissues anchoring gums to teeth. Bacterial toxins break down collagen and supportive proteins, causing gum tissues to pull away from tooth surfaces. This recession is the body’s attempt to remove infected tissue, ultimately exposing tooth roots and compromising the gum’s structural integrity.
Loose Teeth
Prolonged gingivitis leads to systematic destruction of periodontal ligaments and alveolar bone. The continuous bacterial invasion and inflammatory response erode the fundamental support structures holding teeth in place. As these critical tissues break down, teeth lose their stable foundation, resulting in increased mobility and potential misalignment.
These symptoms represent a sophisticated biological response to bacterial invasion. Each sign emerges from a complex interaction between harmful bacteria, the immune system, and oral tissues. The progression demonstrates how an initially minor infection can escalate into a significant oral health challenge.
How to Treat Gingivitis
Effectively addressing gingivitis requires a multifaceted approach that combines professional dental care with comprehensive personal oral health strategies:
Improve Oral Hygiene
Proper oral hygiene forms the cornerstone of gingivitis treatment and prevention. Utilize a soft-bristled toothbrush to minimize gum irritation, paired with fluoride toothpaste that strengthens tooth enamel and fights bacterial growth. Brush thoroughly twice daily, implementing a systematic approach that ensures comprehensive cleaning along the gumline and all tooth surfaces.
Technique is Crucial
Use gentle, circular motions at a 45-degree angle to the gums to effectively remove plaque without causing additional inflammation. Daily flossing is equally critical, as it removes interdental plaque and food particles that toothbrushes cannot reach, preventing bacterial colonization in these hard-to-clean areas.
Use Antiseptic Mouthwash
Antiseptic mouthwashes provide an additional layer of defense against bacterial populations responsible for gingivitis. After brushing and flossing, rinse with an alcohol-free antiseptic mouthwash containing chlorhexidine or essential oils.
These specialized formulations penetrate areas missed by mechanical cleaning, reducing bacterial count and interrupting plaque formation. The antimicrobial agents work to neutralize harmful bacteria, soothe inflamed gum tissues, and create an inhospitable environment for bacterial growth.
Professional Dental Cleaning
Regular professional dental interventions are essential in treating and preventing gingivitis. Dr. Wright can perform thorough dental cleanings that remove stubborn plaque and tartar accumulations impossible to eliminate through home care.
Professional scaling and root planing techniques mechanically remove bacterial buildup, smooth root surfaces, and reduce areas where bacteria can proliferate. These treatments not only address existing gingivitis but also create a clean foundation for improved oral health, allowing gum tissues to heal and reattach to tooth surfaces.
Maintain a Healthy Diet
Nutritional choices play a significant role in gum health and healing. Minimize consumption of sugary and acidic substances that feed harmful bacteria and promote inflammation. Instead, prioritize a balanced nutritional intake rich in vitamins and minerals that support immune function and tissue repair.
Incorporate foods high in vitamin C, which supports collagen production and gum healing, and omega-3 fatty acids, which have natural anti-inflammatory properties. Hydration is equally important, as sufficient water intake helps flush out bacteria and supports overall oral health.
Quit Smoking
Tobacco use severely compromises oral health and immune function, directly impeding gum healing and exacerbating gingivitis. Smoking reduces blood flow to gum tissues, impairs the body’s ability to fight infections, and creates an environment conducive to bacterial growth. Quitting smoking can dramatically enhance oral health, improve immune response, and accelerate gum and tissue regeneration and healing. Patients who quit smoking typically see significant improvements in gum health within weeks of stopping.
Manage Stress
Chronic stress negatively impacts oral wellness by compromising immune function and increasing inflammation. Implement comprehensive stress-management techniques that support both mental and oral health. Regular exercise, meditation, deep breathing practices, and seeking social support can reduce stress hormones that contribute to inflammatory responses. Chronic stress weakens the body’s natural defense mechanisms, making gum tissues more susceptible to bacterial infections and slower to heal.
Regular Dental Checkups
Consistent professional monitoring allows for early detection and personalized treatment guidance. Routine dental visits enable Dr. Wright to track gum health, identify early signs of progression, and implement targeted interventions before gingivitis advances. These checkups provide opportunities for professional cleaning, personalized oral hygiene instruction, and comprehensive assessment of overall oral health.
Gingivitis Treatment Costs
Treatment expenses vary based on condition severity, recommended interventions, and geographical factors. Typical cost estimates include:
- Professional Dental Cleanings: Range from $75 to $200 for routine procedures. Deep cleaning (scaling and root planing) can cost $200 to $400 per mouth quadrant.
- Antibiotic Therapy: Prescription costs depend on specific medications and insurance coverage.
- Additional Treatments: Advanced cases might require specialized procedures like periodontal surgeries or gum grafting, with significantly variable pricing.
Complications of Gingivitis
Untreated gingivitis can lead to a cascade of serious health complications that extend far beyond oral health. When left unchecked, the initial inflammatory response can trigger a destructive process affecting multiple bodily systems:
Periodontal Disease Progression
- Advanced gum disease (periodontitis) develops as inflammation penetrates deeper into oral tissues.
- Bacterial infections destroy the supportive structures around teeth
- Gradual breakdown of periodontal ligaments and alveolar bone occurs
- Increased risk of permanent tooth loss becomes significantly higher
Systemic Health Risks
- Chronic inflammation can contribute to broader health complications
- Potential links to cardiovascular diseases
- Increased risk of diabetes complications
- Potential connections to respiratory infections
- Compromised immune system response
- Higher likelihood of developing inflammatory conditions throughout the body
Dental Structure Deterioration
- Continuous bone loss weakens tooth anchoring
- Gradual recession of gum tissue exposes tooth roots
- Increased tooth sensitivity develops
- Higher susceptibility to dental decay
- Potential misalignment of teeth due to structural changes
Oral Microbiome Disruption
- Harmful bacteria proliferate in infected gum tissues
- Natural protective bacterial balance becomes compromised
- Increased risk of secondary oral infections
- Potential development of chronic bad breath
- Higher chance of developing oral ulcers and lesions
Long-Term Health Implications
- Potential negative impacts on overall systemic health
- Increased inflammatory markers in the body
- Potential contribution to chronic disease development
- Compromised ability of the body to fight infections
- Higher medical treatment costs associated with advanced complications
By understanding these potential complications, patients can recognize the critical importance of early gingivitis intervention and maintaining rigorous oral hygiene practices. Regular dental check-ups and proactive treatment are essential in preventing these serious health risks.
Frequently Asked Questions
Gingivitis is not transmissible between individuals. This bacterial infection develops exclusively through inadequate oral hygiene practices. Consistent plaque removal through proper brushing and flossing is the primary preventative measure. Understanding and implementing comprehensive dental care routines is essential for maintaining optimal oral health.
While personal oral hygiene practices are crucial, professional dental intervention remains necessary for complete treatment. Home care can improve conditions, but professional cleaning addresses hard-to-reach areas impossible to maintain through regular brushing and flossing. Comprehensive dental visits enable thorough plaque and tartar removal, preventing potential progression to periodontal disease.
Gingivitis is indeed reversible with appropriate treatment and improved oral hygiene practices. Early intervention and consistent dental care can completely reverse gingivitis and restore gum health. However, prolonged neglect can transform the condition into periodontitis, causing permanent structural damage to teeth and surrounding tissues.
Prevention centers on establishing robust oral hygiene routines. Brush teeth twice daily using proper techniques, floss at least once daily, and incorporate antiseptic mouthwash. Regular dental checkups and professional cleanings are crucial for monitoring and maintaining optimal oral health. Adopting a holistic approach to dental care significantly reduces gingivitis risk.
Gingivitis represents the initial, reversible stage of gum disease affecting surrounding soft tissues. It results from bacterial plaque accumulation and can be effectively treated with proper intervention. Periodontitis, a more advanced condition, involves bone and structural tissue damage, potentially leading to permanent tooth loss if left untreated.
Gingivitis Doesn’t Stand a Chance Against Our San Clemente Dental Team!
Experiencing gingivitis symptoms like swollen or bleeding gums? Dr. Wright Jr. and our team at Wright Perio & Implants are prepared to help. Serving San Clemente and surrounding areas including Irvine, Laguna Niguel, San Juan Capistrano, and Mission Viejo, we offer personalized, high-quality periodontal care.
Contact us today at (949) 361-4867 to schedule your comprehensive dental evaluation. Take the first step toward a healthier, more confident smile!